Advanced Cardiovascular Life Support (ACLS) is a comprehensive set of clinical interventions designed for the urgent treatment of cardiac arrest, stroke, and other life-threatening medical emergencies. It is an essential skill for healthcare professionals, including physicians, nurses, paramedics, and emergency responders. The primary objective of ACLS is to deliver timely and effective care to patients experiencing cardiac arrest or other cardiovascular emergencies.
ACLS protocols are based on the most recent evidence-based guidelines and are intended to enhance patient outcomes and minimize the risk of complications. ACLS training encompasses a broad range of topics, including basic life support (BLS), airway management, rhythm recognition, pharmacology, and team dynamics. Healthcare providers who undergo ACLS training learn to assess and manage patients in cardiac arrest, as well as recognize and treat various cardiac arrhythmias.
The training also emphasizes the importance of effective communication and teamwork in high-stress situations. By mastering the skills and knowledge taught in ACLS courses, healthcare professionals can significantly improve their ability to respond to cardiovascular emergencies and save lives. ACLS certification is typically valid for two years, after which healthcare providers must undergo recertification to ensure they remain current with the latest guidelines and best practices.
Organizations such as the American Heart Association (AHA) and the American Red Cross offer ACLS courses in both traditional classroom settings and online formats. Healthcare professionals who complete ACLS training gain the confidence and competence to provide advanced care to patients in critical situations, thereby making a significant impact on patient outcomes and survival rates.
Key Takeaways
Identifying and Managing Cardiac Arrest
Cardiac arrest is a life-threatening emergency that occurs when the heart suddenly stops beating, leading to a loss of blood flow to the brain and other vital organs. Prompt recognition and intervention are crucial in managing cardiac arrest and improving patient outcomes. Healthcare providers trained in ACLS are equipped with the knowledge and skills to identify cardiac arrest, initiate cardiopulmonary resuscitation (CPR), and perform advanced interventions such as defibrillation and medication administration.
When managing cardiac arrest, healthcare providers must follow the ACLS algorithms, which provide a systematic approach to resuscitation. The algorithms outline the steps for assessing the patient’s condition, performing CPR, delivering defibrillation shocks, and administering medications such as epinephrine and amiodarone. Effective teamwork and communication are essential during cardiac arrest resuscitation, as multiple healthcare providers may be involved in delivering care to the patient.
In addition to immediate interventions, ACLS also emphasizes post-cardiac arrest care, including targeted temperature management and hemodynamic optimization. By following the latest evidence-based guidelines and algorithms, healthcare providers can improve the chances of successful resuscitation and help patients achieve a positive neurological outcome after cardiac arrest.
Recognizing and Treating Arrhythmias
Cardiac arrhythmias are abnormal heart rhythms that can lead to serious complications, including cardiac arrest and sudden cardiac death. Healthcare providers trained in ACLS are proficient in recognizing and treating various arrhythmias, including atrial fibrillation, ventricular tachycardia, and bradycardia. ACLS courses teach healthcare professionals how to interpret electrocardiograms (ECGs) and identify different types of arrhythmias based on their characteristic waveforms.
Once an arrhythmia is identified, ACLS-trained providers can initiate appropriate interventions based on the specific rhythm. For example, ventricular tachycardia may require immediate defibrillation, while bradycardia may necessitate the administration of atropine or transcutaneous pacing. ACLS also covers the use of antiarrhythmic medications such as amiodarone and lidocaine in managing unstable arrhythmias.
In addition to acute management, ACLS emphasizes the importance of identifying and addressing underlying causes of arrhythmias, such as electrolyte imbalances, ischemia, or drug toxicity. By understanding the pathophysiology of arrhythmias and following evidence-based treatment protocols, healthcare providers can effectively manage these potentially life-threatening conditions and improve patient outcomes.
Utilizing Advanced Airway Management
Advanced airway management is a critical component of ACLS, particularly in patients who require ventilatory support or have a compromised airway. Healthcare providers trained in ACLS are proficient in various airway management techniques, including endotracheal intubation, supraglottic airway insertion, and bag-mask ventilation. ACLS courses teach providers how to assess the need for advanced airway interventions based on the patient’s clinical condition and respiratory status.
When performing endotracheal intubation, healthcare providers must adhere to best practices to ensure successful placement of the endotracheal tube and minimize the risk of complications such as esophageal intubation or hypoxia. Supraglottic airways such as the laryngeal mask airway (LMA) are also valuable tools in managing patients with difficult airways or those who require rapid airway access. In addition to airway interventions, ACLS emphasizes the importance of oxygenation and ventilation in critically ill patients.
Healthcare providers must be skilled in assessing oxygenation status, monitoring end-tidal carbon dioxide levels, and adjusting ventilator settings as needed. By mastering advanced airway management techniques, ACLS-trained providers can ensure adequate oxygen delivery to patients in respiratory distress and improve their chances of survival.
Administering Medications in ACLS
Medication administration is a key aspect of ACLS, as certain medications play a crucial role in managing cardiac arrest, arrhythmias, and other cardiovascular emergencies. Healthcare providers trained in ACLS are knowledgeable about the indications, dosages, and administration routes for various medications used in resuscitation and critical care settings. Common medications used in ACLS include epinephrine, amiodarone, lidocaine, atropine, and vasopressors such as dopamine and norepinephrine.
These medications are administered based on specific algorithms and treatment protocols outlined in ACLS guidelines. For example, epinephrine is indicated in cardiac arrest to improve coronary perfusion pressure and increase the likelihood of successful resuscitation. In addition to medication administration during resuscitation efforts, ACLS also covers the use of antiarrhythmic medications for managing unstable cardiac rhythms.
Healthcare providers must be familiar with the pharmacology of these medications, including their mechanisms of action, potential side effects, and contraindications. By understanding the role of medications in ACLS and adhering to evidence-based guidelines, healthcare providers can optimize patient care during cardiovascular emergencies and improve outcomes for critically ill patients.
Applying Team Dynamics and Communication in ACLS

Effective teamwork and communication are essential components of ACLS, as they play a significant role in coordinating care during high-stress situations such as cardiac arrest resuscitation. Healthcare providers trained in ACLS learn how to function as part of a resuscitation team, communicate effectively with other team members, and delegate tasks based on individual skills and expertise. Team dynamics in ACLS involve clear roles and responsibilities for each team member, including the team leader, airway management provider, chest compression provider, medication administrator, and recorder.
Each team member must be proficient in their respective roles and work together seamlessly to provide coordinated care to the patient. Communication skills are also emphasized in ACLS training, as effective communication is essential for conveying critical information, coordinating interventions, and ensuring a shared mental model among team members. Clear and concise communication helps prevent errors, minimize confusion, and optimize the efficiency of resuscitation efforts.
By mastering team dynamics and communication skills in ACLS, healthcare providers can enhance their ability to work collaboratively in high-pressure environments and improve patient outcomes during cardiovascular emergencies.
Mastering the ACLS Algorithms
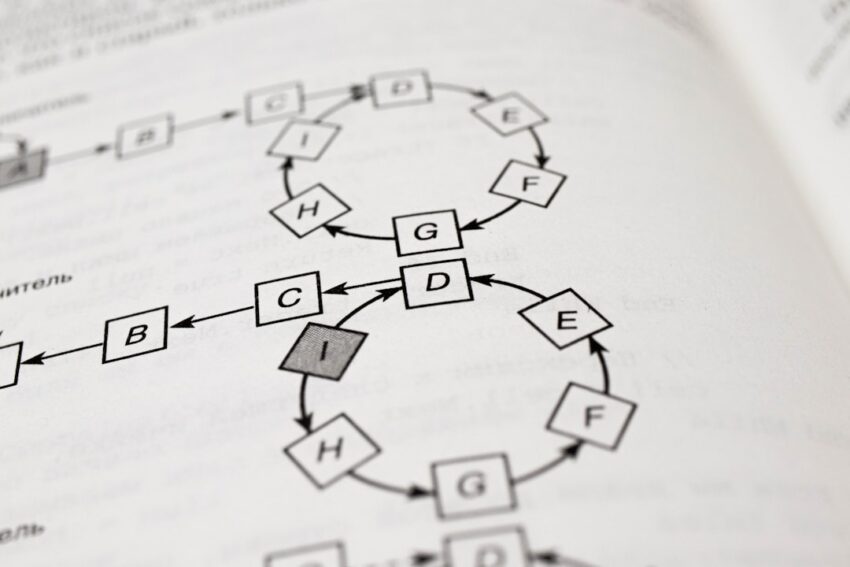
ACLS algorithms provide a systematic approach to managing cardiovascular emergencies by outlining step-by-step protocols for assessment, intervention, and treatment. Healthcare providers trained in ACLS must be proficient in applying these algorithms to various clinical scenarios to ensure timely and effective care for patients in critical condition. The ACLS algorithms cover a range of topics, including adult cardiac arrest, acute coronary syndromes (ACS), bradycardia, tachycardia, pulseless electrical activity (PEA), and asystole.
Each algorithm provides a structured framework for assessing the patient’s condition, performing interventions such as CPR or defibrillation, administering medications, and monitoring response to treatment. By following the ACLS algorithms, healthcare providers can standardize their approach to managing cardiovascular emergencies and improve the consistency and quality of care delivered to patients. The algorithms serve as a valuable resource for decision-making during high-stress situations and help healthcare providers prioritize interventions based on the patient’s clinical presentation.
ACLS certification courses include hands-on practice with simulated scenarios that require participants to apply the algorithms in real-time. This practical experience helps healthcare providers develop confidence in their ability to apply the algorithms effectively when faced with actual patient care situations. In conclusion, mastering the ACLS algorithms is essential for healthcare providers who are responsible for managing cardiovascular emergencies.
By understanding the principles outlined in these algorithms and practicing their application through simulation-based training, healthcare professionals can enhance their readiness to respond to critical situations and improve patient outcomes.
If you’re looking for a comprehensive ACLS study guide, be sure to check out the article “Top 10 Tips for Passing the ACLS Exam” on Imperial Blender. This article provides valuable insights and strategies for successfully preparing for and passing the ACLS exam, making it a valuable resource for anyone studying for this important certification.
FAQs
What is ACLS?
ACLS stands for Advanced Cardiovascular Life Support. It is a set of clinical interventions for the urgent treatment of cardiac arrest, stroke, and other life-threatening medical emergencies.
Who should take an ACLS course?
Healthcare professionals such as doctors, nurses, paramedics, and other medical personnel who may be involved in the management of cardiac arrest and other cardiovascular emergencies should take an ACLS course.
What does an ACLS study guide cover?
An ACLS study guide typically covers topics such as basic life support, advanced cardiovascular life support, airway management, pharmacology, and the management of acute coronary syndromes and stroke.
How can an ACLS study guide help in preparing for the ACLS certification exam?
An ACLS study guide can help individuals review and reinforce their knowledge of ACLS algorithms, medications, and interventions, as well as practice scenarios and case studies commonly encountered in the ACLS certification exam.
Where can I find an ACLS study guide?
ACLS study guides are available from a variety of sources, including online platforms, medical bookstores, and professional organizations that offer ACLS certification courses. It is important to ensure that the study guide is up-to-date and aligned with the latest guidelines from the American Heart Association or other relevant accrediting bodies.